Theme 1 - Mapping Care
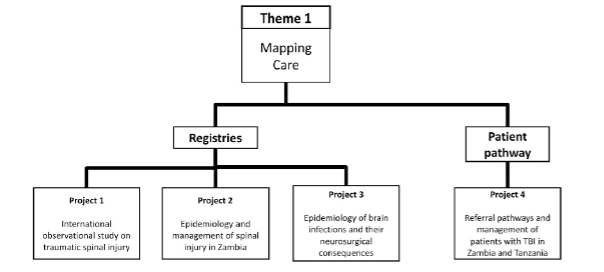
PROJECT 1
What is the epidemiology, management, and outcomes of traumatic spinal injury worldwide?
Project lead:
Background:
The current global approach to the care of patients following traumatic spinal injury (TSI) is inconsistent with considerable geographical differences reported, and limited data available on the impact of these variations on outcomes following TSI.
Aim:
We aim to provide a comprehensive international picture of the management and outcomes of admissions for traumatic spinal injury (TSI) worldwide.
Methods:
A multi-centre, international, prospective observational study. Any unit assessing patients with TSI worldwide will be eligible to participate. Each participating unit will form a study team responsible for gaining local approval, identifying patients for inclusion and conducting data collection. Data will be collected via a secure online platform in an anonymised form. Any primary, secondary or tertiary institution worldwide managing patients with TSI is eligible to participate. In many institutions, management for TSI may be provided by spinal surgeons – however, centres in which management for TSI is provided by general surgeons, trauma surgeons, general medical doctors and non-physician clinicians are also eligible to participate.
Inclusion criteria:
Adult patients presenting to the participating institution with a first presentation of TSI, confirmed radiographically, during the selected 30-day inclusion period are eligible for inclusion in the core study.
Exclusion criteria:
- Elective (planned) or semi-elective (patient initially discharged after emergency with planned intervention at a future date) admissions.
- Patients who have previously had an admission for TSI rendering them eligible for inclusion in this study (regardless of whether they were included on the previous admission or not)
Outcome measures:
Data related to initial presentation, injury management, operative intervention if received, and short-term outcomes will be collected. The dataset, developed through an iterative feedback process involving clinicians from low and high Human Development Index (HDI) countries, includes patient demographics, details of injury mechanism, local injury management and, if applicable, timing and nature of surgery, post-operative care and immediate post-operative complications. The primary outcome measure for this study will be Frankel grade at discharge (or at 30-days following admission, whichever event occurs first).
PROJECT 2
What is the epidemiology, short and long term outcomes of traumatic spinal injury in Zambia?
Project lead:
Background:
The Global Burden of Disease estimated that there were 930,000 new cases of traumatic spinal injury (TSI) (injury to the neurological structures) worldwide in 2016 of which 1,487 were in Zambia(13). Global comparative studies will provide a useful overview of differences in case mix, quality of care and outcomes globally, but truly understanding the challenges to reducing the burden of disease due to TSI requires in-depth local epidemiological research. To our knowledge, no epidemiological studies on TSI in Zambia have been published to date. There is one spinal trauma unit in all of Zambia – based at the University Teaching Hospital (UTH) in Lusaka, staffed by a single fully trained orthopaedic spinal surgeon.
Aim:
To assess epidemiology, management and outcomes of TSI in Zambia.
Methods:
Work Package 1:
Members of the spinal team at UTH will inform the study team when a patient is admitted with TSI. As this project is observational in nature, a sample size calculation is not appropriate. A research assistant will prospectively enter data from TSI patients presenting to UTH into paper-based forms and these will then be transferred to a secure web-based platform. All research staff in Cambridge and Zambia involved in the delivery of the project will be provided with access to the electronic data capture platform, as needed. The data set will include fields on demographics, baseline clinical state and pre-hospital, emergency department, intensive care, surgical and rehabilitation care. All relevant imaging will be reviewed where possible. This aspect of the project will involve data collection only and no changes to routine clinical care will be instituted.
Work Package 2:
Functional outcome and quality of life will be assessed at discharge, 3 months, 6 months, 12 months, 2 years and/or other time points through a combination of telephone calls, clinic appointments and home visits. The assessments will consist of mixed quantitative and qualitative interviews with patients and/or their family members. The exact measures used and the time points listed above at which they are assessed will depend on an initial pilot study assessing feasibility in this population. Ethical approval for the entire project will be sought from the University of Zambia Biomedical Research Ethics Committee, the Zambian National Health Research Ethics Board and the University of Cambridge Humanities and Social Sciences Research Ethics Committee.
Impact:
Understanding the epidemiology, management and outcomes of spine trauma in Zambia will lead to developing designated care pathways and establish the basis for infrastructure and human resource requirements required for sustained improvement.
PROJECT 3
What is the epidemiology of brain infections with neurosurgical complications worldwide?
Project lead:
Background:
Brain infection is a typical disease of poverty. The epidemiology of brain infections and their neurosurgical consequences are virtually unknown(3). It is important to map the disease burden to aid future interventional work.
Aim:
- To undertake an observational study to map the disease burden and presentation of brain infections and their neurosurgical consequences in LMICs, and
- To develop strategies based on improved understanding of injury mechanisms to protect the brain and develop cost-effective health care systems and patient-directed interventions that improve outcome.
Inclusion criteria:
Patients with diagnosed or suspected brain infections (bacterial, tuberculous, parasitic, and malarial origin) and neurosurgical complications (raised intracranial pressure, hydrocephalus, brain ischaemia, mass lesions).
Exclusion criteria:
Patients with no documentation of brain infection. Patients with brain infections without neurosurgical complications.
Methods:
The study will be conducted in centres across Sub-Saharan Africa (South Africa, Zimbabwe, Malawi, Kenya, Nigeria, Ghana, Uganda). We will utilise the CAANS network (Continental Association of African Neurosurgical Societies) of which Anthony Figagi (the joint-lead for this application) is the Education Chair.
Data collected / outcome measures:
We will document the number of cases per treating neurosurgeon (or general surgeon tasked with neurosurgical responsibilities), patient details [age, sex, comorbid disease including HIV, nutritional status, immunizations, etc], the clinical presentation, brain imaging performed and the relevant findings, infectious neurological complications of the disease, treatments delivered, and clinical outcome (as defined by extended Glasgow Outcome Score and Pediatric Extended Glasgow Outcome Score) at hospital discharge (and where available 6 months). We will also gather data on the subject’s primary presentation to healthcare services to ascertain causes of delay in making the diagnosis of brain infections and their consequences.
We will also record infectious pathogens at origin to map the microbiological flora associated with complicated brain infections. The first pass will be onsite with standard basic microbiological techniques available. If funding allows, the second stage will be to collect samples at representative sites, processed and refrigerated locally, and transport the samples to a centre which can perform high level advanced microbiological techniques to detect pathogens at greater sensitivity (as cerebrospinal fluid in postinfectious hydrocephalus may often not reveal the causative pathogen).
We will document the causes of secondary brain injury that lead to worsening of the patients’ neurological condition and the development of neurosurgical complications, including stroke, raised intracranial pressure, hydrocephalus, and mass lesions. We will compare the patterns of disease (presentation, complications, treatments, and outcomes) observed in adults and children to identify age-specific differences in the interplay between infectious pathogen and brain physiology.
We will also compare patterns of disease and microbiological flora with data from cohorts in developed world settings. We will document the training of local neurosurgeons/ general surgeons and skill level in performing the various neurosurgical operations required, what resources for brain monitoring and interventions are used, how these are maintained, and what the needs gap is. Once we have ascertained skill level and access to resources, we will embark on training in basic neurosurgical skills for managing the neurosurgical complications of brain infections.
Future work:
Once we have mapped the disease and the skill level of the available surgeons, we will examine how cost-effective interventions may change local management of patients with respect to earlier diagnosis (e.g. the use of transfontanelle ultrasound in young children, transorbital ultrasound, transcranial Doppler, noninvasive cerebral oximetry, and biomarkers. Local surgeons will undergo training in these techniques at selected sites as a pilot project to collect preliminary data in the first year (discovery). Thereafter, where funding allows, the most promising technique(s) will be generalised across more centres (validation).
At selected centres we will embark on novel studies if funding allows. These include:
- The application of blood-based biomarkers for early diagnosis, disease tracking, and prognostication
- Penetration of antimicrobial drugs into the central nervous system to determine the factors that influence this (including type of drug, drug dose, route of administration, patient factors [eg nutritional status, liver function], and underlying pathology [eg. loculations in hydrocephalus, the blood brain barrier].
PROJECT 4
For patients with traumatic brain injury, how does the referral pathway from a district general hospital to a tertiary hospital function?
Project lead:
Background:
A key concept central to the management of traumatic brain injury (TBI) is that only part of the injury occurs at the time of trauma (primary injury), while the rest evolves over the ensuing hours and days (secondary injury). Emergency medical services, which include first responders, ambulance crew and staff in Emergency Departments in district hospitals are therefore central to the management of TBI. Data from LMICs suggests that patients transferred to neurosurgical units for definitive care from neighbouring hospitals have much larger delays to receiving care (14) but little information exists on the reasons for these delays and the care pathways and quality of care these patients receive.
Aim:
To assess the care of patients with TBI referred from district general hospitals to neurosurgical units in Tanzania and Zambia.
Methods:
Work Package 1: We will prospectively include all patients admitted to participating neurosurgical units in Dar es Salaam, Tanzania and Lusaka, Zambia with TBI over a 1-year period. Mode of transportation to hospital, initial management, time to imaging, time to referral and time to transfer will be evaluated. Both patients transferred from other hospitals and those admitted directly to a neurosurgical unit will be included and the two groups compared. Long term outcome will be sought.
Work Package 2: A cross-sectional survey of resources available for the management of TBI in a sample of first, second and third level hospitals in Tanzania and Zambia will be undertaken. A survey will first be designed and piloted in select institutions. An up to date list of first, second and third level hospitals will be obtained from the respective country’s Ministry of Health. Senior clinicians at selected hospitals will be contacted by phone, e-mail or SMS and asked to complete a paper-based or online survey examining the capacity for the management of TBI at their institution. Where no response is obtained from an institution, a formal site visit will be undertaken by a Clinical Research Fellow. Province Medical Directors will be contacted and requested to aid with the dissemination of the survey to appropriate clinicians at each health facility meeting the inclusion criteria in their province. Questions will pertain to pre-hospital, emergency department, intensive care, surgical and rehabilitative management in each institution and its surrounding catchment area. Work Package 3: A Clinical Research Fellow or research assistant will undertake site visits to a sample of first, second and third level hospitals in Tanzania and Zambia in order to conduct qualitative, semi-structured interviews about the quality of care of TBI in district general hospitals. Staff members at each institution will be selected from a sample of pre-hospital, emergency department, surgical, intensive care and rehabilitative care providers. A subset of patients who have participated in Work Package 1 will be invited to participate in this aspect of the study as well. Qualitative interviews and data collection will continue until data reaches a level of redundancy at which point analysis of the data will begin. Ethical approval will be sought from the necessary committees.
Impact:
Understanding the principles of managing TBI in district general hospitals will lead to developing designated care pathways and establishing reliable links between initial healthcare providers and the definitive treatment facilities. This will include training in, and resource provision for initial resuscitation and stabilisation, as well as, providing infrastructure to aid rapid diagnosis and communication with the definitive treatment centres if such exist.